Update: 7/14/2020: While some here have disputed that nutrition could play a significant role in fighting COVID-19, a new study points to Vitamin D as a key factor. See “Vitamin D levels appear to play role in COVID-19 mortality rates” at ScienceDaily.com.
Update: 4/2/2020: An important new study explains why glucosamine may be an effective aid in coping with the Corona virus, as well as other nutraceuticals such as N-acetyl cysteine, sulforophane (found in broccoli and other cruciferous vegetables), spirulina and selenium (high in Brazil nuts, but don’t take too much because this essential nutrient can be carcinogenic in excess). While the publication is in a peer-reviewed journal, it is not based on original clinical work but reviews numerous related studies and pulls together bits and pieces to offer a hypothesis that such nutriceuticals may be effective in coping with influenza and the Corona virus. It may not do any good, but there is little harm to making sure you have broccoli and a few Brazil nuts in your diet, and both glucosamine and N-acetyl cysteine are already popular nutriceuticals that are low in toxicity and known to have some benefits. However, I’ve also seen studies warning that excess anti-oxidants like N-acetyl cysteine can also increase cancer risk since our body’s defenses against cancer cells often can involve oxidative reactions that can be hindered when anti-oxidants are too high. However, N-acetyl cysteine is well known as a treatment for cystic fibrosis because it reduces the viscosity of the biofilm mucous in the lungs, so using it for COVID-19 doesn’t seem like an outrageous stretch. I am not a medical expert so get advice from competent sources before you do anything unusual based on the new publication See M.F. McCarty and J.J. DiNicolantonio, “Nutraceuticals have potential for boosting the type 1 interferon response to RNA viruses including influenza and coronavirus,” Progress in Cardiovascular Diseases (in press, available online Feb. 12, 2020), https://doi.org/10.1016/j.pcad.2020.02.007. Here is an excerpt from the report:
Glutathione production can also be promoted by administration of N-acetylcysteine (NAC), which has been shown to be protective in rodents infected with influenza.16., 17., 18. In a little-noticed 6-month controlled clinical study enrolling 262 primarily elderly subjects, those receiving 600 mg NAC twice daily, as opposed to those receiving placebo, experienced significantly fewer influenza-like episodes and days of bed confinement.19 Although the rate of seroconversion to influenza A was comparable in the two groups – indicating that they were exposed at the same frequency – only 25% of the virus-infected subjects in the NAC group developed symptoms, as contrasted to 79% of those of placebo. (Given the carnage that influenza wreaks among the elderly, it is most regrettable that no effort has been made to replicate this study, conducted over 20 years ago.) The particular utility of NAC in the elderly might reflect the fact that plasma cysteine levels and cellular glutathione levels tend to decline with advancing age.20
Update, 2/29/2020: In light of helpful and competent feedback to me privately about the problems in the proposed mechanisms for the hypotheses examined here and about the weaknesses in some of the studies mentioned (e.g., lack of real clinical data), there is no compelling reason to believe that dietary factors have a clear effect on the mortality of COVID-19, or that glucosamine can reduce pneumonia mortality, though it may be possible. Given that some non-clinical published studies point to positive effects of glucosamine in lung-related matters, there may be a valid need for further research on the topic, but no need to insist that glucosamine should be shipped to China or to claim that significant dietary changes will have a strong impact. There’s still the possibility that it might help in treating pneumonia from SARS-CoV-2, but large question marks remain, especially regarding proposals that certain foods and drinks may impact mortality.
For those interested in exploring the currently speculative role of glucosamine in lung health, the original post below will remain in place, but recognize that serious question marks remain in place about the proposal discussed therein.
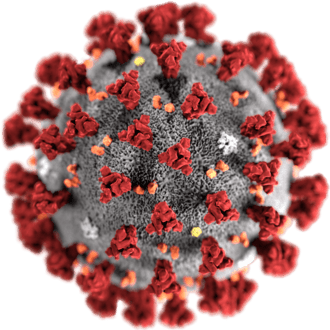 |
| Illustration of a SARS-CoV-2 virion,
courtesy of the CDC. |
In response to recent posts about the impact of the Corona virus, now known as SARS-CoV-2 and its disease, COVID-19, on China and the Church (especially my branch and district in Shanghai), I was pleased to be contacted by one of my readers, C.T., who shared tentative findings from her investigation of factors that may affect how severe pneumonia can become in once healthy patients. She posted some information on this blog, leading to the some of the pointed criticism that is normally reserved for me. She has not granted permission to use her name, but given the hostility she encountered from trolls when she posted her work originally on her own blog, I can understand a desire to remain anonymous. But I find her proposal interesting enough and, if correct, potentially valuable enough that I’d like to invite feedback from competent experts to see if there is any merit and if further work is warranted. If C.T.’s work could help alleviate some of the suffering that COVID-19 is causing, and specifically decrease the mortality rate, that would be fantastic. Or, like much of the output of creative thinkers and researchers, maybe it’s just an interesting idea that in the end won’t prove to be fruitful. Let’s see.
In presenting some tentative possibilities below, please note that I am not making any medical claims or suggesting that nutrition or nutritional supplements can directly reduce the risk of dying from COVID-19 or pneumonia in general. I am not seeking to spread rumors about the disease (spreading rumors is strictly illegal in China, especially rumors or incorrect information about sensitive issues such as COVID-19 and its management, and as one who loves so much about China and its people, and still has an apartment there, I strive to abide by the regulations), but am inviting experts to review a tentative possibility that could be helpful to China and other nations. I also have no financial interest in this matter (apart from having an apartment and other things China made much less accessible by the severity of COVID-19, all of relatively minor importance to me).
C.T.’s hypothesis involves the possible role of glucosamine and other aspects of nutrition in reducing the risk of severe pneumonia. Glucosamine is a natural material found in cartilage and in the shells of shrimp, crabs, etc. and the skeletons of marine animals. Perhaps offering an especially practical opportunity for China, it is also present in China’s abundant and delicious mushrooms and other fungi (see “Dietary Sources” below). It is an antioxidant that our body can produce, though it is also commonly sold as a dietary supplement said to help treat osteoarthritis and reduce pain in joints (see an overview of reports on glucosamine at ScienceDirect). In what follows, I’ll add some comments to C.T.’s points and mix a few finds from my searching with some of the things she has found.
The relationship between glucosamine and cartilage health has a reasonable basis (though for relieving pain, as the BBC reports, it’s not clear that glucosamine supplements actually do more than a good, full-strength placebo), and cartilage is present in several vital parts of the lungs, from the trachea through the bronchi. C.T.’s hypothesis is that viral disease may infect chondrocytes, cells that product cartilage, and that our own immune system in response may then attack those cells and lead to tissue damage that allows naturally present bacteria to cause severe infection. But could there be a relationship between glucosamine and pneumonia mortality? C.T. proposes a mechanism involving the SOX-9 protein and its role in driving a “cytokine storm” where dangerous cycles can lead to severe illness. She argues that dietary influences that inhibit or enhance the effect of SOX-9 (i.e., down regulate or up regulate) may help explain significant differences in pneumonia mortality among nations, with tea and perhaps pomegranate juice being likely to up regulate SOX-9 while diets high in shrimp and cartilage may provide the glucosamine that can may regulate SOX-9. You can see her recent comments on the Coronavirus and the crisis in Wuhan in her post of Jan. 31, 2020, “My two bits about the novel coronavirus from Wuhan,” which points to her earlier post with the key information she wishes to share. [Update, 2/28/2020: Shortly after I posted this information, the links to her blog and to her YouTube video below went dead. I have since learned that she has taken down that information today. I am puzzled about why and recognize that it raises troubling questions when a researcher doesn’t want to be associated with their work. I don’t know her reasons, but perhaps it is a privacy issue related to the harsh treatment she received when she originally posted her tentative findings.]
Whether or not C.T.’s proposed mechanisms and dietary considerations are correct, there are peer-reviewed studies suggesting that glucosamine may help reduce mortality from respiratory illness. If so, that could be helpful information for afflicted people.
The scientific literature on glucosamine tends to focus on its role in cartilage formation and in alleviating problems with joints and bones. But there are some surprising finds related to other effects. Here are a few to consider (the first and fourth were pointed out by C.T. in her original work):
1. Griffith A. Bell et al., “Use of glucosamine and chondroitin in relation to mortality,” European Journal of Epidemiology, 27/8 (2012): 593-603; https://www.jstor.org/stable/23272500.
Abstract: Glucosamine and chondroitin are products commonly used by older adults in the US and Europe. There is limited evidence that they have anti-inflammatory properties, which could provide risk reduction of several diseases. However, data on their long-term health effects is lacking. To evaluate whether use of glucosamine and chondroitin are associated with cause-specific and total mortality. Participants (n = 77,510) were members of a cohort study of Washington State (US) residents aged 50-76 years who entered the cohort in 2000-2002 by completing a baseline questionnaire that included questions on glucosamine and chondroitin use. Participants were followed for mortality through 2008 (n = 5,362 deaths). Hazard ratios (HR) for death adjusted for multiple covariates were estimated using Cox models. Current (baseline) glucosamine and chondroitin use were associated with a decreased risk of total mortality compared to never use. The adjusted HR associated with current use of glucosamine (with or without chondroitin) was 0.82 (95 % CI 0.75-0.90) and 0.86 (95 % CI 0.78-0.96) for chondroitin (included in two-thirds of glucosamine supplements). Current use of glucosamine was associated with a significant decreased risk of death from cancer (HR 0.87 95 % CI 0.76-0.98) and with a large risk reduction for death from respiratory diseases (HR 0.59 95 % CI 0.41-0.83). Use of glucosamine with or without chondroitin was associated with reduced total mortality and with reductions of several broad causes of death. Although bias cannot be ruled out, these results suggest that glucosamine may provide some mortality benefit. [Emphasis added. For links to references cited by Bell et al., see the Springer page for this article.]
2. Kun-Han Chuang et al., “Attenuation of LPS-induced Lung Inflammation by Glucosamine in Rats,” American Journal of Respiratory Cellular Molelcular Biology, 49/6 (Dec. 2013): 1110-9.
Abstract: Acute inflammation is often observed during acute lung injury (ALI) and acute respiratory distress syndrome. Glucosamine is known to act as an anti-inflammatory molecule. The effects of glucosamine on acute lung inflammation and its associated mechanisms remain unclear. The present study sought to address how glucosamine plays an anti-inflammatory role in acute lung inflammation in vivo and in vitro. Using the LPS intratracheal instillation-elicited rat lung inflammation model, we found that glucosamine attenuated pulmonary edema and polymorphonuclear leukocyte infiltration, as well as the production of TNF-α, IL-1β, cytokine-induced neutrophil chemoattractant (CINC)-1, macrophage inflammatory protein (MIP)-2, and nitric oxide (NO) in the bronchoalveolar lavage fluid (BALF) and in the cultured medium of BALF cells. The expression of TNF-α, IL-1β, IFN-γ, CINC-1, MIP-2, monocyte chemotactic protein-1, and inducible NO synthase (iNOS) in LPS-inflamed lung tissue was also suppressed by glucosamine. Using the rat alveolar epithelial cell line L2, we noted that the cytokine mixture (cytomix)-regulated production and mRNA expression of CINC-1 and MIP-2, NO production, the protein and mRNA expression of iNOS, iNOS mRNA stability, and iNOS promoter activity were all inhibited by glucosamine. Furthermore, glucosamine reduced LPS-mediated NF-κB signaling by decreasing IκB phosphorylation, p65 nuclear translocation, and NF-κB reporter activity. Overexpression of the p65 subunit restored the inhibitory action of glucosamine on cytomix-regulated NO production and iNOS expression. In conclusion, glucosamine appears to act as an anti-inflammatory molecule in LPS-induced lung inflammation, at least in part by targeting the NF-κB signaling pathway.
3. Yuh-Lin Wu et al., “Glucosamine Attenuates Cigarette Smoke-Induced Lung Inflammation by Inhibiting ROS-sensitive Inflammatory Signaling,” Free Radical Biology and Medicine, 69 (April 2014): 208-18; DOI: 10.1016/j.freeradbiomed.2014.01.026.
Abstract
Cigarette smoking causes persistent lung inflammation that is mainly regulated by redox-sensitive pathways. We have reported that cigarette smoke (CS) activates a NADPH oxidase-dependent reactive oxygen species (ROS)-sensitive AMP-activated protein kinase (AMPK) signaling pathway leading to induction of lung inflammation. Glucosamine, a dietary supplement used to treat osteoarthritis, has antioxidant and anti-inflammatory properties. However, whether glucosamine has similar beneficial effects against CS-induced lung inflammation remains unclear. Using a murine model we show that chronic CS exposure for 4 weeks increased lung levels of 4-hydroxynonenal (an oxidative stress biomarker), phospho-AMPK, and macrophage inflammatory protein 2 and induced lung inflammation; all of these CS-induced events were suppressed by chronic treatment with glucosamine. Using human bronchial epithelial cells, we demonstrate that cigarette smoke extract (CSE) sequentially activated NADPH oxidase; increased intracellular levels of ROS; activated AMPK, mitogen-activated protein kinases (MAPKs), nuclear factor-κB (NF-κB), and signal transducer and activator of transcription proteins 3 (STAT3); and induced interleukin-8 (IL-8). Additionally, using a ROS scavenger, a siRNA that targets AMPK, and various pharmacological inhibitors, we identified the signaling cascade that leads to induction of IL-8 by CSE. All these CSE-induced events were inhibited by glucosamine pretreatment. Our findings suggest a novel role for glucosamine in alleviating the oxidative stress and lung inflammation induced by chronic CS exposure in vivo and in suppressing the CSE-induced IL-8 in vitro by inhibiting both the ROS-sensitive NADPH oxidase/AMPK/MAPK signaling pathway and the downstream transcriptional factors NF-κB and STAT3.
4. Jean-Noël Gouze et al., “Exogenous glucosamine globally protects chondrocytes from the arthritogenic effects of IL-1β,” Arthritis Research and Therapy, 8 (2006), article #R173; https://doi.org/10.1186/ar2082. (PDF also available.)
Abstract
The effects of exogenous glucosamine on the biology of articular chondrocytes were determined by examining global transcription patterns under normal culture conditions and following challenge with IL-1β. Chondrocytes isolated from the cartilage of rats were cultured in several flasks either alone or in the presence of 20 mM glucosamine. Six hours later, one-half of the cultures of each group were challenged with 10 ng/ml IL-1β. Fourteen hours after this challenge, RNA was extracted from each culture individually and used to probe microarray chips corresponding to the entire rat genome. Glucosamine alone had no observable stimulatory effect on the transcription of primary cartilage matrix genes, such as aggrecan, collagen type II, or genes involved in glycosaminoglycan synthesis; however, glucosamine proved to be a potent, broad-spectrum inhibitor of IL-1β. Of the 2,813 genes whose transcription was altered by IL-1β stimulation (P > 0.0001), glucosamine significantly blocked the response in 2,055 (~73%). Glucosamine fully protected the chondrocytes from IL-1-induced expression of inflammatory cytokines, chemokines, and growth factors as well as proteins involved in prostaglandin E2 and nitric oxide synthesis. It also blocked the IL-1-induced expression of matrix-specific proteases such as MMP-3, MMP-9, MMP-10, MMP-12, and ADAMTS-1. The concentrations of IL-1 and glucosamine used in these assays were supraphysiological and were not representative of the arthritic joint following oral consumption of glucosamine. They suggest, however, that the potential benefit of glucosamine in osteoarthritis is not related to cartilage matrix biosynthesis, but is more probably related to its ability to globally inhibit the deleterious effects of IL-1β signaling. These results suggest that glucosamine, if administered effectively, may indeed have anti-arthritic properties, but primarily as an anti-inflammatory agent.
5. Ji-Sun Hwang et al., “Glucosamine Improves Survival in a Mouse Model of Sepsis and Attenuates Sepsis-Induced Lung Injury and Inflammation,” Journal of Biological Chemistry, 294/2 (Jan. 11, 2019): 608-622; DOI: 10.1074/jbc.RA118.004638.
Abstract
The aim of the current study was to investigate the effects of glucosamine (GlcN) on septic lethality and sepsis-induced inflammation using animal models of mice and zebrafish. GlcN pretreatment improved survival in the cecal ligation and puncture (CLP)-induced sepsis mouse model and attenuated lipopolysaccharide (LPS)-induced septic lung injury and systemic inflammation. GlcN suppressed LPS-induced M1-specific but not M2-specific gene expression. Furthermore, increased expressions of inflammatory genes in visceral tissue of LPS-injected zebrafish were suppressed by GlcN. GlcN suppressed LPS-induced activation of mitogen-activated protein kinase (MAPK) and NF-κB in lung tissue. LPS triggered a reduction in O-GlcNAc levels in nucleocytoplasmic proteins of lung, liver, and spleen after 1 day, which returned to normal levels at day 3. GlcN inhibited LPS-induced O-GlcNAc down-regulation in mouse lung and visceral tissue of zebrafish. Furthermore, the O-GlcNAcase (OGA) level was increased by LPS, which were suppressed by GlcN in mouse and zebrafish. OGA inhibitors suppressed LPS-induced expression of inflammatory genes in RAW264.7 cells and the visceral tissue of zebrafish. Stable knockdown of Oga via short hairpin RNA led to increased inducible nitric oxide synthase (iNOS) expression in response to LPS with or without GlcN in RAW264.7 cells. Overall, our results demonstrate a protective effect of GlcN on sepsis potentially through modulation of O-GlcNAcylation of nucleocytoplasmic proteins.
In light of these studies, especially the first one, there seems to be some reason to believe that glucosamine may be helpful in reducing the mortality of pneumonia. If so, and that’s still a definite “if” demanding further research and review, being prepared to have a diet with some glucosamine sources or to have some glucosamine on hand might be reasonable should COVID-19 become a serious threat in your community, or if you are traveling under conditions where you may be exposed to the SARS-CoV-2 virus. Your intelligent feedback on this is welcome — but anonymous trolling comments that I too often tolerate will be deleted here in order to increase the chance of readers finding intelligent comments that help us better understand the issues raised here.
C.T.’s Proposals on Mechanism and Diet
C.T. posted the following note on my blog a couple days ago:
Hi, Jeff, I know it sounds presumptuous, but I think I figured out which environmental triggers are involved in making it so people exposed to this virus do/do not become symptomatic and how severe the symptoms are.
1) Damage to the hyaline cartilage (by the immune system targeting infected cartilage cells) is much less likely to happen where the diet contains glucosamine (in shrimp paste and cartilage), where there is no exposure to dry and cold air, and where there is not bleach being sprayed in the air (seriously, have Hubei’s bureaucrats never heard of chemical pneumonia?).
2) The cartilage cells, if damaged, think they have to rebuild the hyaline cartilage matrix and so secrete chondroitin sulphate and other cartilage matrix molecules; the gene SOX9 is very instrumental in doing this, but if it is overly active it can cause there to be too many such molecules building up in the lungs. Voila! Viral pneumonia. What gets SOX9 going? EGCG appears to “stimulate exuberant cartilage matrix secretion” (see https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4247298/), and EGCG is THE special molecule in tea leaves. What did the poor people of Wuhan ingest in their apartment quarantines: rice, veggies, legumes, and tea–no meat or shrimp. What else affects SOX9? Turmeric (curcumin decreases SOX9 activity–lucky Thailand), Fluoride (also helps decrease SOX9 activity–lucky India), Pomegranate (increases SOX9–unlucky Iran, where they drink pomegranate juice when sick). This hypothesis holds up even in Italy, where they drink wine and coffee all the time except when they’re trying to lose weight or fight a cold–then they drink green tea. And it utterly refutes all the stupid internet trolls who were going on and on about how “Chinese people have horrible hygiene.”
Doctrine & Covenants 89 is a beautiful piece of counsel for our times.
C.T.’s original post on the relationship between glucosamine and mortality in pneumonia and the possible mechanisms involved is “Glucosamine to protect cartilage during influenza infection,” Petticoat Government, Feb. 5, 2018. (Sadly, her blog and her YouTube video were taken down the day this was posted, as noted above.) Here is an excerpt with the key arguments she makes:
1) The flu infects chondrocytes, the cells in cartilage. They are the only cells in hyaline cartilage, which type of cartilage is coincidentally found in places–joints, rib ends, nose, larynx, trachea, bronchi–that are among the hardest hit by influenza. (https://www.britannica.com/science/cartilage)
2) Influenza-infected chondrocytes don’t seem to actually experience obvious damage until the body’s immune system goes on the attack. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC422866/; http://onlinelibrary.wiley.com/doi/10.1046/j.1365-2567.2003.01621.x/full) [Edited 2/17/2018: Someone pointed out to me that chondrocytes are within an extracellular matrix that has no blood vessels, so other cells, including attacking immune cells, can’t reach them. I looked more into that issue and found a 2015 cartilage transplant study which found that cartilage isn’t as immune-privileged as it used to be believed it was (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4522233/). I suspect that chondroblasts–the immature chondrocytes next to the blood-vessel-containing perichondrium–are the first chondrocytes which the immune system cells attack, and then due to their destruction the cartilage matrix becomes compromised; if that compromised state becomes severe enough, immune cells can then gain access to the mature chondrocytes within, as well.]
3) Cytokines are part of the immune system’s attack arsenal. The cytokine IL-1beta is a critical component of lung inflammation during infection with influenza type A H1N1. (http://onlinelibrary.wiley.com/doi/10.1002/jmv.24138/abstract; https://www.ncbi.nlm.nih.gov/pubmed/27714503)
4) Glucosamine–a natural compound found in cartilage–happens to protect chondrocytes by being a potent inhibitor of IL-1beta. (https://link.springer.com/article/10.1186/ar2082)
5) Damaged cartilage in the trachea/bronchi could allow for more penetrating infection by viruses/bacteria that normally would not be able to do much harm and in that way make flu sufferers much more susceptible to pneumonia. Most of the people who died from the 1918 flu died because “bacteria that normally inhabit the nose and throat invaded the lungs along a pathway created when the virus destroyed the cells that line the bronchial tubes and lungs.” (https://www.nih.gov/news-events/news-releases/bacterial-pneumonia-caused-most-deaths-1918-influenza-pandemic)
6) People who take glucosamine (it’s a common supplement for arthritis) are much less likely to die of respiratory illnesses than their peers. (https://link.springer.com/article/10.1007/s10654-012-9714-6)
So if you’re worried about influenza, it might be worth it to buy some glucosamine and take it when you’re exposed to influenza so you can protect your hyaline cartilage and thus make yourself less likely to develop pneumonia….
Eat well cooked, or non-manufactured source- glucosamine rich foods (like shrimp) to help the cartilage stay strong, and stay away from tea plant and pomegranate for a second. (Pomegranates are healthy, but are rich in natural SOX9 stimulants… Which is good… But on a viral, over-production level ((what happens with this virus)) you get to much in the lungs too fast, and therefore pneumonia.)
There is also a related video on YouTube made before COVID-19 came along. [Update: Sadly, this was taken down, with her blog, shortly after this post. Sorry!]
By the way, I have worked with nearly pure EGCG as part of my consumer products research work in the past and was often surprised by how reactive it is. Dissolve a little white EGCG in water and combine with baking soda or other alkaline material and find out what strange, ugly stains you can create on materials such as tissue paper or fabrics after allowing it to sit for a few hours. It has many effects in the body, some clearly positive, but I can imagine that there are situations where this reactive material isn’t helpful. Can it play the role that C.T. suggests? I don’t know, but would like to learn more. Is it possible that giving tea to the ill might not be a good idea? I don’t know, but it may not be helping in Wuhan, though so much of what’s happening there remains opaque. If you have additional useful information, please let me know.
Dietary Sources
C.T. points to shrimp as an important dietary source of glucosamine. I should add that it appears that the glucosamine of shrimp comes from the shell, not the flesh. In Asia, many people eat the shells, or so it seems to me, especially small shrimp where the shell is quite thin and, in fried shrimp, can be tasty and easy to eat. She also mentions gristle, which is commonly consumed, especially chicken gristle. Another source may be soups in which the bones of animals have been stewed for a long period of time. Bone-rich soup, at least in China, especially when stewed long enough to create a white broth, is widely held to be very nutritious and ideal for those who are ill, and probably supplies some glucosamine. I find it delicious, too.
There are also options for vegetarians. Mushrooms contain chitin, the widespread natural polymer found in the shells of shrimp, crabs, insects, etc., and glucosamine is one of the building blocks of chitin and I believe it can be released when digested. See Tao Wu et al., “Chitin and Chitosan–Value-Added Products From Mushroom Waste,” Journal of Agricultural Food Chemistry, 52 /26 (Dec. 29, 2004): 7905-10; DOI: 10.1021/jf0492565. Also see Pin Zhang et al., “Kinetic Models for Glucosamine Production by Acid Hydrolysis of Chitin in Five Mushrooms,” International Journal of Chemical Engineering, 2020, article ID 5084036 (2020); https://doi.org/10.1155/2020/5084036.
Unfortunately, for those in Wuhan, there are reports that the diet is now necessarily simple and thus there may be less meat (bone and cartilage included) and less shrimp than usual, so the protective effects of glucosamine, if real, may be less available than normal. C.T. worries that the combination of cold, stress, and confinement, coupled with a low-glucosamine and high-tea diet and even the occasional exposure to bleach or other harsh chemicals in the effort to kill the virus in many places might make a perfect storm for elevated pneumonia risk for those infected with the virus. If C.T.’s proposal is correct, then bringing glucosamine or glucosamine-rich foods to Wuhan and other affected areas may be a helpful step to help reduce loss of life.
One of China’s great blessings when it comes to food is the richness of its fungi, with numerous wild and domesticated mushrooms and other fungi that are so delicious. Some are far too expensive for me, but there are many varieties that are relatively inexpensive but very nutritious, especially the black wood ear fungus called mu er (literally wood ear). It’s more expensive than rice or common vegetables like carrots, onions, or cabbage, but it’s still quite cheap and has also been touted for its immune strengthening benefits. I order some much of the time when I’m in Chinese restaurants in China. Perhaps adding this to the diet of the people in Wuhan and other afflicted cities could help?
Is Glucosamine Safe for Those Allergic to Shrimp?
Finally, one important issue is whether those with seafood allergies, including shellfish allergies, should take glucosamine since it is often made from the shells of shrimp. Please consult with your physician and don’t take crazy risks based on random bloggers. However, something to consider as you discuss such matters with competent medical authorities is that several studies suggest that commercially available high-quality glucosamine may not contain the allergens that are harmful to some people. Here are a couple studies to consider:
J. Villacis et al., “Do Shrimp-Allergic Individuals Tolerate Shrimp-Derived Glucosamine?,” Clinical and Experimental Allergy, 36/11 (Nov. 2006): 1457-61; DOI: 10.1111/j.1365-2222.2006.02590.x.
Abstract
Background: There is concern that shrimp-allergic individuals may react to glucosamine-containing products as shrimp shells are a major source of glucosamine used for human consumption.
Objective: The purpose of this study was to determine whether shrimp-allergic individuals can tolerate therapeutic doses of glucosamine.
Methods: Subjects with a history of shrimp allergy were recruited and tested for both shrimp reactivity via a prick skin test and shrimp-specific IgE by an ImmunoCAP assay. Fifteen subjects with positive skin tests to shrimp and an ImmunoCAP class level of two or greater were selected for a double-blind placebo-controlled food challenge (DBPCFC) using glucosamine-chondroitin tablets containing 1,500 mg of synthetically produced (control) or shrimp-derived glucosamine. Immediate reactions, including changes in peak flow and blood pressure, and delayed reactions (up to 24 h post-challenge) via questionnaire were noted and assessed.
Results: All subjects tolerated 1,500 mg of both shrimp-derived or synthetic glucosamine without incident of an immediate hypersensitivity response. Peak flows and blood pressures remained constant, and no subject had symptoms of a delayed reaction 24 h later.
Conclusion: This study demonstrates that glucosamine supplements from specific manufacturers do not contain clinically relevant levels of shrimp allergen and therefore appear to pose no threat to shrimp-allergic individuals.
Heather C. Gray, et al., “Is glucosamine safe in patients with seafood allergy?,” Jounral of Allergy and Clinical Immunology, 114/2 (August 2004) 459–460; DOI: https://doi.org/10.1016/j.jaci.2004.05.050 (PDF also available).
Excerpt:
Six subjects participated in the study. All 6 had a history consistent with a systemic reaction to shellfish. All 6 had positive skin prick test responses to shrimp, crab, lobster, or a combination of these. All 6 had negative skin test responses to the glucosamine extract (Table I) and uneventful oral challenges with glucosamine, with no change in skin, vital signs, or spirometry….
Approximately 600 patients must be recruited to ensure that the chance of rejecting an allergy rate of at least 0.5% is less than 0.05. This pilot study, which indicates that glucosamine is probably safe for patients with shellfish allergy, emphasizes the need for further investigation, with larger studies looking at different shellfish allergens and the consistency of glucosamine formulations.
Further research is needed on this issue and others raised above. If you have other information on the food safety issue or other issues raised here, please share. Thanks!
I welcome your feedback, but I will be deleting more anonymous trolling comments than I normally do because I would like the comments to be helpful. But to save the usual trolls the trouble, let me just jump the gun and recognize that yes, I am not trained in medicine or the life sciences and, as usual, am daring to offer thoughts that are amateur and worthy of ridicule. Ridiculous, absurd, idiotic, and a blight on humanity. There, done! Your non-anonymous criticisms are welcome, though, if they contribute to the quest to understand what measures we can take to reduce the mortality of COVID-19 or to help people prepare for the risks it may bring.
Other Related Resources:
Theodore M. Brasky, “Use of Glucosamine and Chondroitin and Lung Cancer Risk in the VITamins And Lifestyle (VITAL) Cohort,” Cancer Causes and Control, 22/9 (Sept. 2011): 1333-42. See also Theodore M. Brasky et al., “Long-term use of glucosamine and chondroitin and lung cancer risk in the vitamins and lifestyle (VITAL) cohort,” Cancer Research, 71/8 (April 2011), DOI: 10.1158/1538-7445.AM2011-1912.
Jody Braverman, “Nutritional Value of Bone Gristle,” LiveStrong.com, September 30, 2019.
“Glucosamine sulfate,” WebMD, https://www.webmd.com/vitamins/ai/ingredientmono-807/glucosamine-sulfate. (Information on possible benefits, risks, interactions with other drugs, etc.)
Hao Ma et al., “Association of habitual glucosamine use with risk of cardiovascular disease: prospective study in UK Biobank,” BMJ 365 (May 14, 2019); DOI: https://doi.org/10.1136/bmj.l1628. (Potential benefits in preventing cardiovascular disease.)
Robert H. Shmerling, “The latest on glucosamine/chondroitin supplements,” Harvard Health Blog, Oct. 17, 2016.
“Too much glucosamine can cause the death of pancreatic cells, increase diabetes risk, researchers find,” ScienceDaily.com, October 27, 2010.
L.H. Toledo-Pereyra et al., “Lung Transplantation: Better Survival Results After Graft Pretreatment With Concanavalin A or Chondroitin Sulfate,” Annals of Thoracic Surgery, 29/3 (March 1980): 209-16; DOI: 10.1016/s0003-4975(10)61869-3.
Update A, 2/28/2020: There’s one study C.T. mentioned suggesting that chondroitin, which is often combined with glucosamine in supplements, can cause pneumonia rather than prevent it, based on a single patient. See Takeshi Satomura et al., “A Case of Drug-induced Pulmonary Disease Considered to be Caused by a Supplement Containing Chondroitin,” The Journal of the Japan Society for Respiratory Endoscopy, 37/2 (2015): 214-18; DOI https://doi.org/10.18907/jjsre.37.2_214.
Abstract
Drug-induced pulmonary disease can be caused by a variety of drugs including supplements. We examined a case of drug-induced organizing pneumonia induced by a supplement containing chondroitin. Case. An 80-year-old man had been taking supplements for knee pain since early July 2013 and subsequently developed a cough and fever. A chest radiograph demonstrated infiltrative shadows, and he was admitted to our hospital. His condition did not improved with antibiotic treatment and bronchoscopy was performed for diagnostic purposes. A transbronchial lung biopsy specimen showed organizing pneumonia, and the patient’s condition was ameliorated with steroid therapy. We established a diagnosis of drug-induced pulmonary disease based on the results of a lymphocyte stimulation test for a supplement containing chondroitin. Conclusions. We conclude that the use of supplements containing chondroitin may result in drug-induced pulmonary disease.
That single case may not be meaningful, but if you’re concerned and want more glucosamine after consulting with medical personnel, you can just use glucosamine alone or a diet with glucosamine. Chondroitin tends to me relatively more expensive anyway. Consult your physician and don’t rely on bloggers.
Update B, 2/28/2020: One physician whom I deeply respect weighed in on this and said the link between SOX-9 and pneumonia seems very tenuous. He also fears that the proposed relationship to tea and pneumonia mortality may not be driven by data but by a bias in favor of the Word of Wisdom. Those are reasonable responses.
As for the area that seems stronger to me, the possible link between glucosamine and respiratory illness, his view is that the studies were observational rather than carefully designed which can lead to bias and other distortions. Later after looking more carefully, he observed that there wasn’t any data from a clinical setting that would support the idea of taking glucosamine to prevent or treat pneumonia. Further, he noted that pneumonia involves inflammation of the alveoli, not the cartilage in the bronchi. And he observed that SARS-CoV-2 infects epithelial cells almost exclusively, which does not fit her model. If there is merit to any of the proposals discussed above, further research and clarification is needed.
I also took a look at the article linking EGCG to SOX-9 and cartilage growth, and agree that there’s a big gap in the alleged link between drinking tea and being more likely to die from pneumonia. The ability of SOX-9 to encourage cartilage growth still isn’t clearly connected to the lung tissue damage seen in COVID-19 patents. It’s a tenuous link, but is not the key to C.T.’s core proposal regarding glucosamine.
Update C, 2/28 & 2/29/2020: The unexpected closing of C.T.’s blog and the YouTube video after this post was frustrating, though I have since learned that she has a valid reason related to privacy, though I don’t know the details. But I can’t argue against those who say that it doesn’t bode well for research when the researcher won’t be or can’t be named and withdraws related publications. In spite of that problematic issue, I still want to be open minded to see if there might be merit to the proposals C.T. has made. However, feedback already suggests there may be some flaws in both the theory and the interpretation of some studies. So far it looks like the intriguing theory and proposal may not as promising as I hoped, but still might have value. Further work may be needed. Given the low risk of taking glucosamine, I might keep some around just in case. But I hope I don’t have the opportunity to be part of a trial on surviving COVID-19, and also hope that none of you will have that opportunity (but likewise hope that all of you survive it you are infected).





One quick question. Can you name one other infectious disease that is greatly influenced by diet (ie: mortality rates are affected by consumption or deletion if certain foods)?
Good question. First, remember that C.T. is making no claim about diet affecting the spread of the SARS-CoV-2 virus, but rather the severity of pneumonia. But to your point, while dietary factors play a big role in many noninfectious diseases and certainly can have all sorts of complex effects on the body, it does seem unusual to me that a disease like pneumonia might be so directly affected by diet.
There's a general review article on diet and infectious disease, but it's doesn't have anything as dramatic as C.T.'s proposal: Sedigheh Farhadi and Roman S Ovchinnikov, "The relationship between nutrition and infectious diseases: A review," Biomedical and Biotechnology Research Journal, 2/3 (2018): 167-72.
I look forward to further input on this issue. I don't know enough, obviously.
Of course, given that there is some clinical data linking glucosamine to respiratory health and mortality, and since glucosamine intake is related to our diet or to dietary supplements, our unawareness of dietary relationships for other diseases may not be particularly meaningful. Your thoughts?
So why is the death toll attributed to Corona virus and not pneumonia?
When one looks at research on specific dietary components such as vitamins, there can be a mix of studies proposing some linkage in alleviating, preventing, or exacerbating infectious disease. One example is Vitamin A: see "Vitamin A Supplementation, Infectious Disease and Child Mortality: A Summary of the Evidence,"
Nestle Nutrition Institute Workshop Series, 2012. But I would appreciate input from experts in this area.
Jeff you're just copy/pasting nonsense based off of anonymous comments. Why are you doing this? It's flagrantly dangerous. You aren't an expert. This isn't your field. You likely don't even understand what you've posted. This isn't helping.
Dangerous to seek professional feedback on a proposal about a possible low-risk means of reducing the impact of pneumonia based? Dangerous to encourage discussion and feedback on some peer-reviewed publications pointing to a potentially positive role of a low-cost, natural material that might be helpful, or might be worth further research to see if it is actually applicable to COVID-19? Even if glucosamine does not help much, what is the harm of this exercise in seeking feedback? And if it does help, can you imagine that there might be harm in ignoring the potential aid?
Why am I doing this? I have numerous friends at risk because of this virus. A nation I love is suffering, other nations that I care about are being afflicted, and the U.S. that I deeply love may soon be at risk. I see evidence that COVID-19 is spreading rapidly in Asia and beyond, and that it is being sorely mismanaged in the US (hardly anyone being tested because of CDC errors, quarantines being bungled, infected patients brought back on planes contrary to CDC recommendations, data already being ordered to be controlled and censored, etc. — not boding well for robust, effective protection). Can we avoid widespread harm from this virulent disease that is quite different than the flu? I hope so, but we may need better ways to prepare. If dietary factors can increase our odds of survival against pneumonia, let's explore that while we wait for vaccines. What's the harm you worry about? I've been careful to explain that I am looking for answers, not giving them, but there are some hints in the literature that C.T.'s suggestion may have a touch of merit, in spite of big questions marks about C.T.'s mechanisms.
Of course I'm not an expert. But I do track information on this virus carefully and do understand at least some of the references I've provided. There's a lot about transcription factors like SOX-9 I don't get, and it's not clear to me that chondrocytes are actually infected by the virus and attacked by the immune system, nor why that would lead to problem of pneumonia, and maybe it doesn't. Since I'm not an expert, that's why I'm asking for intelligent input, not just the usual trolling comments of anonymous critics.
The goal is to help. This is an unusual post, I admit, but if the thoughts shared can stir anyone to consider additional, practical ways to help deal with the outbreak, it will be worth the effort. Can you explain why discussing this topic will do more harm than potential good? Granted, it might if glucosamine were toxic and terribly expensive, or if glucosamine were known to increase pneumonia mortality, but I don't think those factors are at play here.
The goal is to help and you are failing, no matter what your intent may be. There's already way too much noise on the issue.
Too much noise on the issue of glucosamine and lung health? Or too much noise on how to reduce the risk of death by Corona virus? What sources are you turning to with too much noise on these issues?
What if glucosamine does help reduce mortality from pneumonia, as at least one peer-reviewed study suggests? If that is the case, can you explain why raising that possibility as a topic for further research or consideration is not helpful?
Oh, wait, you're anonymous. You can say anything without the least accountability or impact on your reputation. OK, no need to reply. I get it.
We may as well be asking if aspirin can prevent coronavirus. Or if ibuprofen can prevent AIDS. Can Pepto prevent Alzheimer's? Can essential oils prevent cancer? I'M JUST ASKING THE QUESTIONS HERE!
Jeff, you have complete control over whether or not people can comment anonymously here. You know that, right?
"We may as well be asking if aspirin can prevent coronavirus." Oh, so there's a peer-reviewed study linking aspirin intake to surviving respiratory disease? If not, then there's quite a difference.
In fact, aspirin was a cause of death for the Spanish flu, when the U.S. government, influenced by a big pharma company seeking to profit from the disease, made a terrible recommendation to take very high aspirin levels to treat the flu, levels that today are known to be well above the maximum safe limit. See the New York Times article, "In 1918 Pandemic, Another Possible Killer: Aspirin." In fact, one peer-reviewed study suggests that high aspirin intake, driven by the US government's irresponsible recommendation, may have been a major contributor to the high mortality rate in that dreadful pandemic. See Karen M. Starko, "Salicylates and Pandemic Influenza Mortality, 1918–1919: Pharmacology, Pathology, and Historic Evidence," Clinical Infectious Diseases, Volume 49, Issue 9 (15 November 2009): 1405–1410, DOE: doi.org/10.1086/606060.
Has the reliability of information from the US government become significantly greater over time? Or is it still improperly influenced by big money, sometimes to our detriment? Do your own diligence, but I don't think that we can always trust what government officials say.